Interpretation of post-transplant related (lung) complications is mainly and initially
done on hematoxylin and eosin stained slides. In the revised ISHLT Working Formulation
for lung rejection, AMR was recognized as an important clinical entity (1).
The Pathology Council of the ISHLT has recently proposed a summary
statement on the pathology of AMR after lung transplantation.
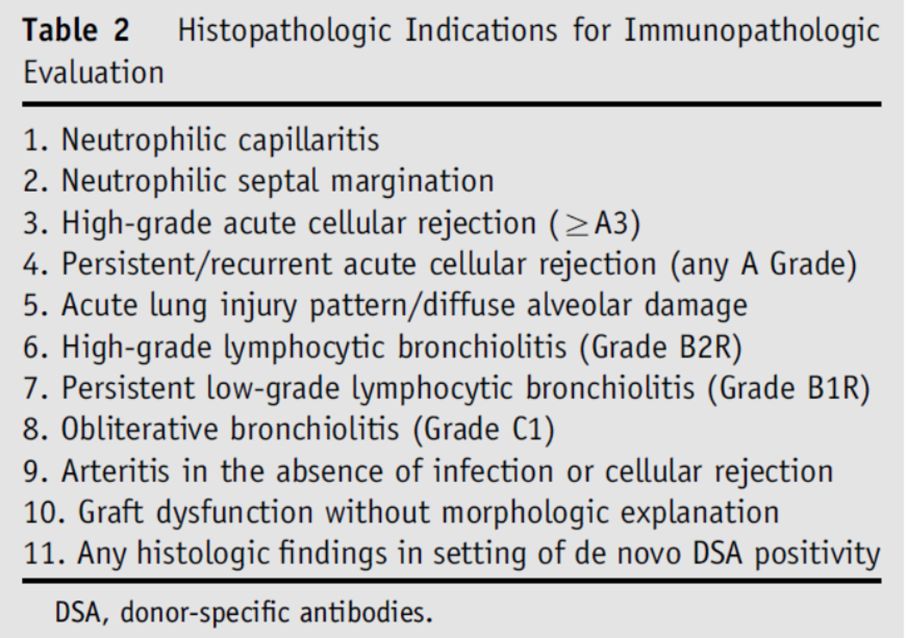
The main histopathological findings are reported in the Table 2 of the consensus statement.
The list of histopathologic patterns associated with AMR is sufficiently
broad to suggest that unless the lung biopsy is normal, then AMR should be considered.
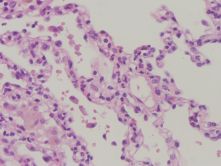
Capillary inflammation, acute lung injury with endothelial swelling and fibrin leakage
(in severe cases) and endothelitis have been reported significantly correlated with
DSA positive AMR (Figure 1) (2,3).
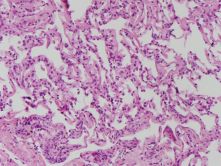
The AMR web tutorial working group, during work meeting,
confirmed the frequent occurrence of capillaritis and other lung injury together with
new some aspects (broading alveolar septa with mononuclear infiltration) (Figure 2)
that must be confirmed revising other cases during our multidisciplinary work meetings.
However this histologic picture is not specific; further support can be found by delicate
immunohistochemical presence of C4d (see Immunohistochemistry). Considering the broad
differential diagnosis, confirmation has to be sought by demonstration of pathological
levels of anti-HLA/non anti-HLA antibodies; notably, even when a patient does not show
specific symptoms at that time.
Pitfalls
Recent evidence has highlighted capillary inflammation, acute lung injury
and endothelitis as correlated with DSAs and consequently with AMR (3).
These lesions however could be detected in many other lung injuries such as
ischemia/reperfusion damage, infection, drug toxicity, aspiration pneumonia,
severe acute cellular rejection and autoimmune disorders.
Thus the above mentioned pathological features may be suggestive of AMR
after careful investigation and exclusion of other etiologies.
Wim Timens (Pathologist, University of Groningen, NL)
References :
1. Stewart S, Fishbein MC, Snell GI, Berry GJ, Boehler A, Burke MM, Glanville A, Gould FK, Magro C, Marboe CC, McNeil KD, Reed EF, Reinsmoen NL, Scott JP, Studer SM, Tazelaar HD, Wallwork JL, Westall G, Zamora MR, Zeevi A, Yousem SA. Revision of the 1996 working formulation for the standardization of nomenclature in the diagnosis of lung rejection. J Heart Lung Transplant 2007; 26:1229-1242.
2. Berry G, Burke M, Andersen C, Angelini A, Bruneval P, Calabrese F, Fishbein MC, Goddard M, Leone O, Maleszewski J, Marboe C, Miller D, Neil D, Padera R, Rass D, Revello M, Rice A, Stewart S, Yousem SA. Pathology of pulmonary antibody-mediated rejection: 2012 update from the Pathology Council of the ISHLT. J Heart Lung Transplant. 2013 Jan;32(1):14-21.
3. Wallace WD, Li N, Andersen CB, Arrossi AV, Askar M, Berry GJ, DeNicola MM, Neil DA, Pavlisko EN, Reed EF, Remmelink M, Sam WS, Weynand B, Zhang JQ, Budev MM, Farver CF. Banff study of pathologic changes in lung allograft biopsy specimens with donor-specific antibodies. J HeartLung Transplant 2016; 35:40-48.