AMR is a well-accepted entity in both kidney and heart allografts.
The diagnosis in both the kidney and heart allograft is suspected based on the combination
of the presence of graft dysfunction, circulating DSA and pathological and
immunologic-pathologic changes. There is a considerable amount of evidence
in the literature recognizing the association between DSA’s with allograft rejection,
decreased graft survival and poorer outcomes in both of these organ systems.
The diagnosis of pulmonary AMR, however, has been especially complex and difficult to make.
Although there is a recognized association between DSAs and acute and chronic allograft
dysfunction, it has been a challenge to make a specific diagnosis.
Up until now, there have been no standardized diagnostic criteria or an agreed upon definition.
This made it difficult to diagnose pulmonary AMR, interpret individual cases or create
management and therapeutic guidelines. Recently, a working group of the ISHLT established
a set of standardized diagnostic criteria in order to better define and diagnose pulmonary AMR.
The creation of these criteria is a big step forward in the identification of pulmonary AMR.
It gives us a uniform base to start from when trying to recognize and diagnose this entity.
It is based on the Banff Criteria, AMR is in both the kidney and heart. However,
the nonspecific nature of the pathologic features in lung tissue, the issues with the
reliability of C4d staining as a marker for complement activation in the lung, as well
as the overlap of clinical signs and symptoms with other lung pathologies, continue to
make the diagnosis challenging. Uniform use of these standardized criteria as well as further
characterization of this entity will help to guide future changes to the definition.
Below is the summary of the criteria established in the ISHLT consensus statement (1).
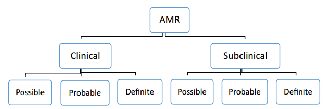
Staging of Pulmonary AMR:
AMR may be defined as either clinical or sub-clinical:
1. Clinical AMR:
The presence of allograft dysfunction associated with AMR. Clinical AMR may
be asymptomatic, such as a small but significant change in pulmonary physiology.
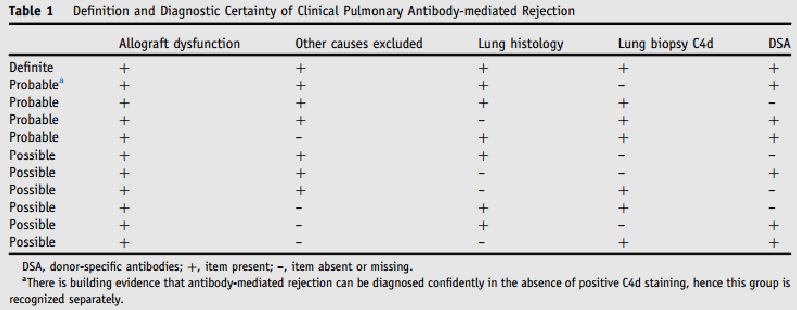
(a) Definite clinical AMR: Allograft dysfunction in the presence of DSA plus
positive histology suggestive of AMR and positive C4d staining.
ACR and AMR can be concurrent, but other causes have been excluded.
(b) Probable clinical AMR: Allograft dysfunction in the presence of 2
of the 3 following criteria: presence of DSA; positive histology suggestive of AMR;
and positive C4d staining. A grading of probable AMR may be given to a recipient who
has coexistent AMR with infection or ACR when all 3 diagnostic criteria are present.
(c) Possible clinical AMR: Allograft dysfunction in the presence of 1 of 3 following criteria:
presence of DSA; positive histology suggestive of AMR; and positive C4d staining.
A grading of possible AMR may be given to a recipient who has coexistent AMR with
infection or ACR when 2 diagnostic criteria are present.
It was agreed that idiopathic allograft dysfunction may, in some cases,
be due to a form of AMR not yet characterized.
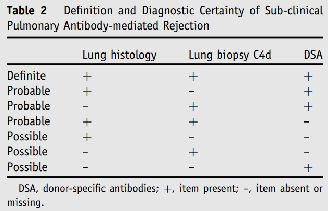
2. Sub-clinical AMR:
Histologic criteria of AMR detected on surveillance transbronchial biopsies
(with or without C4d and with or without the presence of DSA)
in the absence of allograft dysfunction.
Classification of Pulmonary AMR based on the presence (clinical) or absence
(sub-clinical) of allograft dysfunction, and confidence of diagnosis (1).
Definition and Diagnostic Certainty of Clinical Pulmonary AMR (1)
Definition and Diagnostic Certainty of Sub-clinical Pulmonary AMR (1)
Deborah Jo Levine (Transplant Pulmonologist, University of Texas Health Science Center, USA)
References :
1. Levine et al. “ISHLT Consensus Report: Antibody-mediated rejection of the lung: A consensus report of the International Society for Heart and Lung Transplantation”. J Heart Lung Transplant 2016;35:397–406.